CHALLENGES
• Expand the practice into a surgery center
• Streamline operations
• Billing conducted in-house
• Gaps in practice management system
• Backlog of 120+ accounts receivable
PROCESS
• Alerted practice on coding changes and denial trends
• 100% patient eligibility two days and authorizations five days prior to the Date of Service
• Insurance follow-up within 15 days of claims submission
• Billed claims within 24-hours of service
• Partnered with the practice to build corporate website and improve marketing and online presence
• Consulted and tracked center’s Meaningful Use compliance
• Co-ordinated with collection agency of the center for collecting patient balances
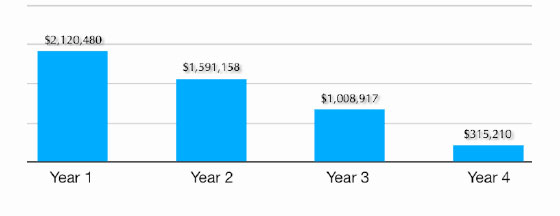
RESULTS
• Collections increased by $500,000 upon transition
• Global agreement negotiated for anesthesia providers at 92% of fee schedule
• Transitioned practice to a web based practice management system, conducted onsite training
• Reconciled old Medicare claims worth $50,000
• Practice successfully expanded into a surgery center
• Center was able to collect $60,000 as Meaningful Use incentives
“With healthcare reform looming, we look forward to growing together”